
[ad_1]
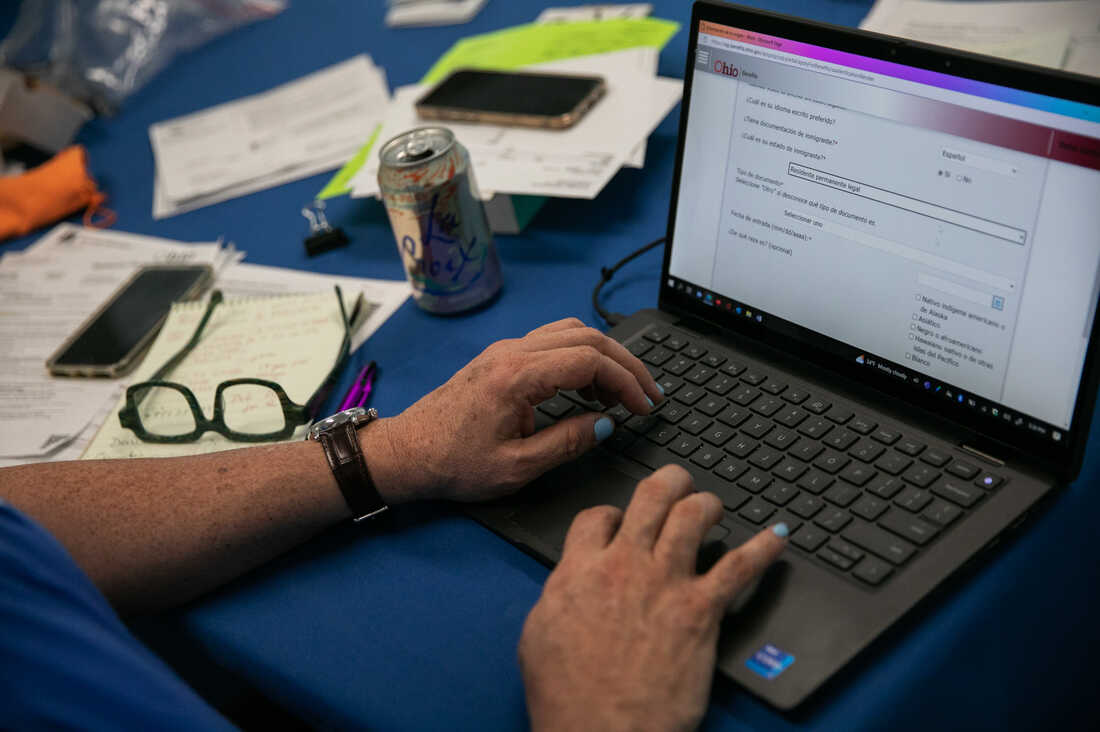
Samuel Camacho, a medical insurance navigator with the Common Well being Care Motion Community of Ohio, assists folks in enrolling for or renewing Medicaid.
Maddie McGarvey for NPR
conceal caption
toggle caption
Maddie McGarvey for NPR
Samuel Camacho, a medical insurance navigator with the Common Well being Care Motion Community of Ohio, assists folks in enrolling for or renewing Medicaid.
Maddie McGarvey for NPR
Dominique Jackson has been on Medicaid for seven years. However the Columbus, Ohio, resident did not notice he’d must confirm his eligibility yearly to maintain his protection. Then, he sprained his ankle.
“I discovered that I needed to re-enroll as a result of I went to the emergency room and I nonetheless had my previous Medicaid card. And once they scanned it, it got here up that I used to be not underneath that supplier,” Jackson recollects. Fortunately, he was in a position to work file the paperwork and get his care lined.
For the previous three years, Jackson and tens of thousands and thousands of different Individuals on Medicaid have not needed to fear about retaining their protection. That is as a result of early within the pandemic, Congress handed a legislation that prevented states from dropping folks from their Medicaid rolls.
“That is been actually enormous, since you do not need to discover out that you do not have your Medicaid whenever you’re within the emergency room, particularly throughout a pandemic,” says Kathryn Bamberger, who heads up a group of medical insurance navigators at Southeast Healthcare, a well being middle serving low-income sufferers all through central Ohio.
This was one large motive behind traditionally excessive charges of Medicaid enrollment and an all-time low fee of people that have been uninsured within the U.S. final 12 months.
However these protections expire on March 31, which implies that as of April 1, states can as soon as once more start eradicating folks from their Medicaid rolls. Estimates counsel that nationwide, between 15 million and 18 million folks are susceptible to shedding their Medicaid protection over the approaching months.
That features almost 7 million individuals who stay eligible for this system however face limitations to filling out their paperwork in a well timed method, in keeping with projections from the Division of Well being and Human Companies.
The renewal course of “goes to hit everybody within the Medicaid program,” says Jennifer Tolbert, affiliate director for this system on Medicaid and the uninsured on the Kaiser Household Basis.
However it will not occur suddenly. Tolbert says states have some leeway in how they restart the signup course of. Nearly all of states plan to do it over a 12-to-14-month interval, in keeping with a report from KFF.

Camacho frequently units up a desk on the public library to assist folks with Medicaid enrollment. He says little errors in paperwork can result in denials within the enrollment course of.
Maddie McGarvey for NPR
conceal caption
toggle caption
Maddie McGarvey for NPR

Camacho frequently units up a desk on the public library to assist folks with Medicaid enrollment. He says little errors in paperwork can result in denials within the enrollment course of.
Maddie McGarvey for NPR
That might assist what’s certain to be a messy and tough course of. Re-enrolling is riddled with obstacles for enrollees – beginning with the actual fact they might not even obtain the notification that they should do it, and together with difficulties in acquiring the sorts of documentation required to show their eligibility.
Preventing by way of a maze of paperwork
Ohio is one in every of eight states that started the renewal course of in February, in keeping with KFF, and it has already began sending out renewal notices. However Bamberger says folks on Medicaid typically get disenrolled, even when they’re nonetheless eligible, as a result of the state cannot attain them they usually by no means reply to requests for verifications of family dimension or earnings.
“You have bought a disproportionate variety of folks right here who aren’t laptop literate and whose housing is unstable,” Bamberger says, including, “Simply because I listed my buddy as a mailing tackle three years in the past does not imply that that particular person’s going to maintain my mail in order that I can get it now if I am homeless. [Or] what if that tackle is on your previous girlfriend or boyfriend, and you have not spoken in two years?”
She notes that verifying paperwork might be difficult to get in case your job does not present a pay stub otherwise you work within the gig economic system – for instance, as a driver for DoorDash. “They get their fee data on their cellphone. It does not seem like a pay stub that someone who’s working [a traditional] job in an workplace will get.”
Stephanie Jorgensen has skilled this irritating course of firsthand. “Gathering all the verifications is like essentially the most nerve-racking half. It is a job,” she says.
Jorgensen lives in Columbus, Ohio. She’s spent a lot of her profession working in social providers nonprofits. She’s additionally a single mom of two on Medicaid, and is at the moment unemployed whereas ending a certification in graduate college. But regardless of her experience, she says it is a ton of labor to navigate the system.
“I’ve a masters diploma and it is nonetheless like a struggle each step of the way in which,” she says.
For instance, Jorgensen has to supply documentation that she not works at a nonprofit that she left greater than a decade in the past, which has since closed up store. “I am unable to even get a verification from them stating that they do not exist,” she says.
Nonetheless, Jorgensen is comparatively fortunate. No less than she is aware of she has to resume her Medicaid quickly. Nearly all of Individuals enrolled in Medicaid do not know they’re going to must act to maintain their protection, in keeping with a survey launched in February by the City Institute.
Most states are conducting outreach campaigns to encourage Medicaid recipients to replace their tackle data, in keeping with KFF. However Bamberger says the truth is, many individuals will not notice they’ve misplaced Medicaid protection till they really want it.
“We absolutely anticipate in April for folks to name us from the pharmacy,” Bamberger says. “That is typically the place they study that, ‘Oh, my Medicaid does not work.”
Navigators assist overcome language limitations
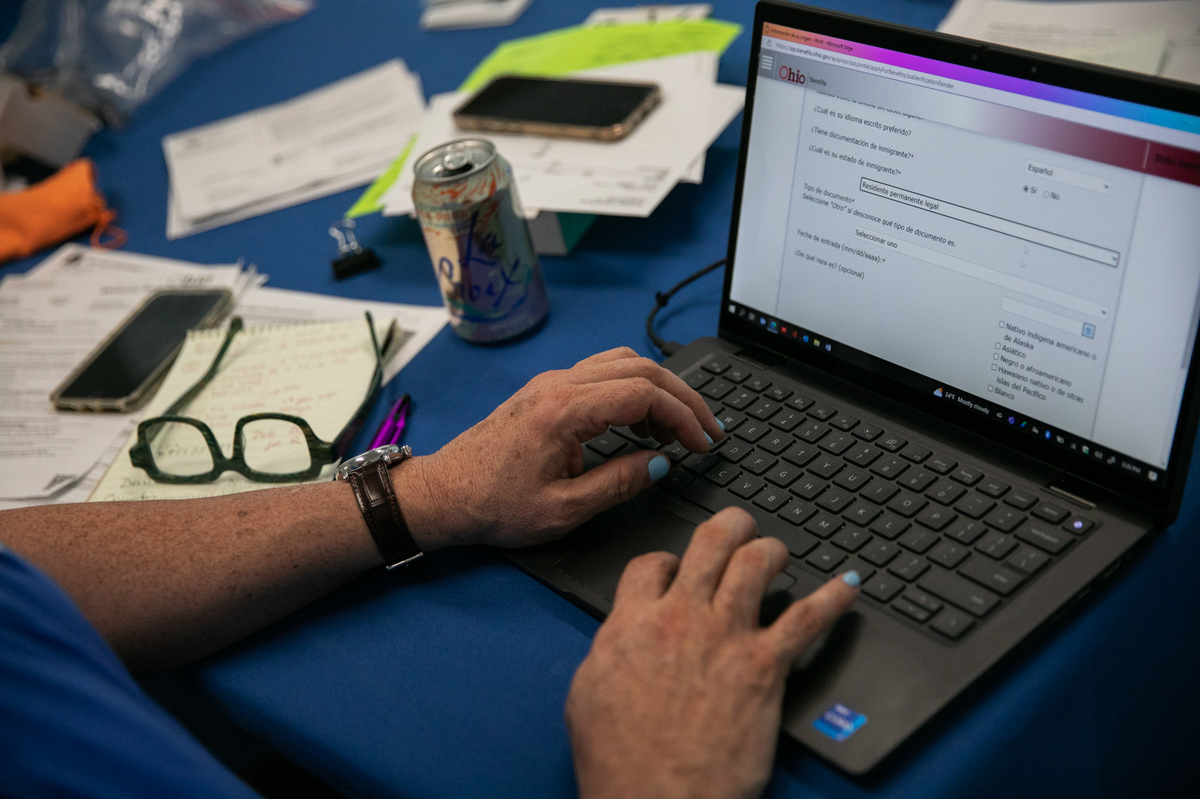
Samuel Camacho, a medical insurance navigator with the Common Well being Care Motion Community of Ohio, says language is one other main barrier. “People are going to be weak due to their lack of English. So they might obtain a letter, however they cannot learn it,” he says. Navigators like Camacho information folks in signing up for Obamacare, however they’ll additionally help them with Medicaid.

Camacho says phrase of mouth is actually essential for the Latino neighborhood he works with. He helps Spanish audio system, typically moms, with Medicaid enrollment over the cellphone or at public libraries.
Maddie McGarvey for NPR
conceal caption
toggle caption
Maddie McGarvey for NPR

Camacho says phrase of mouth is actually essential for the Latino neighborhood he works with. He helps Spanish audio system, typically moms, with Medicaid enrollment over the cellphone or at public libraries.
Maddie McGarvey for NPR
Camacho helps Spanish audio system within the Columbus, Ohio, area. He says the method has gotten a lot tougher, as a result of the native workplaces for the company that handles Medicaid have been closed to the general public for the reason that pandemic.
“Earlier than the pandemic, people have been in a position to go to the workplaces with an interpreter and have conversations with their case managers, print paperwork, discover paperwork of their language, have interactions with folks, even different Medicaid recipients. We have misplaced that,” Camacho says.
He says that sort of phrase of mouth is actually essential for the Latino neighborhood he works with. “Latinos – we’re a gaggle that thrives on communication. ‘Abuelita le dijo a Titi, Titi le dijo al primo y el primo me lo dijo a mi.’ [Grandma told auntie, auntie told the cousin, and the cousin told me.] So we’re shedding that.”
These days, Camacho helps Spanish audio system, typically moms, with Medicaid enrollment over the cellphone or at public libraries. He says the method typically takes two hours. However that is simply the beginning of it. He says he typically has to interpret when the state sends requests for extra documentation.
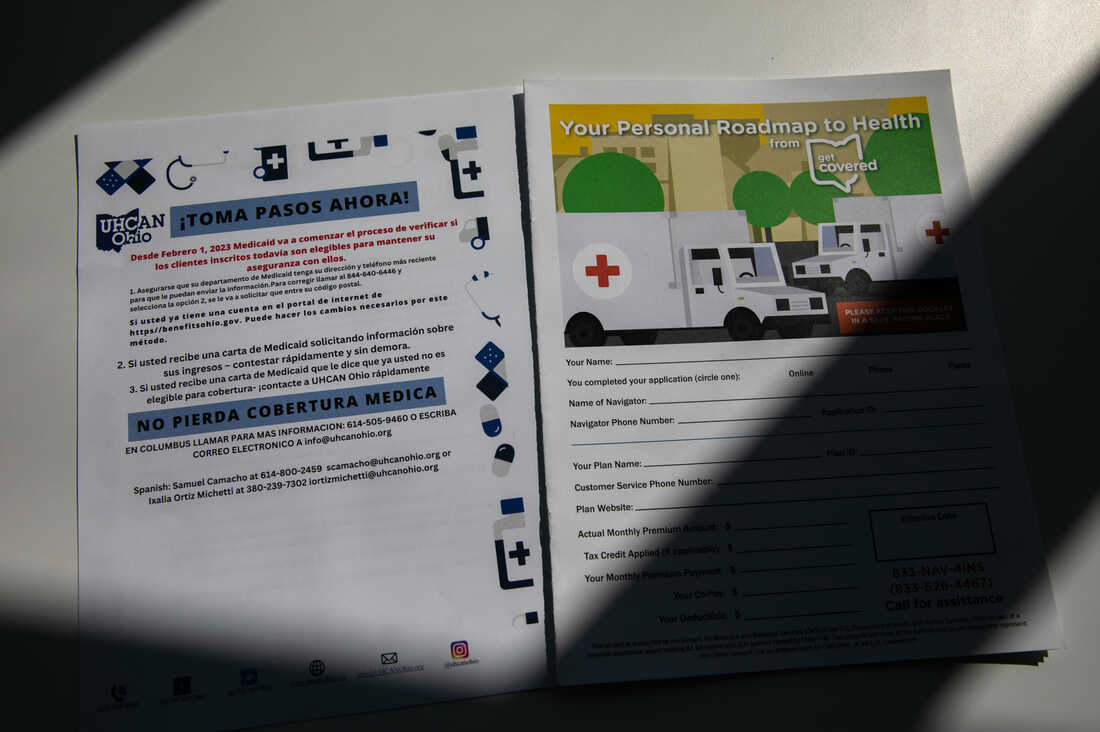
Camacho says he needs to verify everybody on Medicaid is aware of they should re-enroll within the coming months.
Maddie McGarvey for NPR
conceal caption
toggle caption
Maddie McGarvey for NPR

Camacho says he needs to verify everybody on Medicaid is aware of they should re-enroll within the coming months.
Maddie McGarvey for NPR
For instance, he stated, an individual may submit a invoice underneath their partner’s identify, nevertheless it must be underneath each their names. “Little particulars. And if these particulars aren’t taken care of, you are denied,” he says.
Camacho says in his expertise, these denials occur as a rule. And regardless that they’re normally overturned on attraction, “it is the heartache of getting to do it repeatedly and once more. Is not sensible.”
As irritating as it may be, Camacho says he needs to verify everybody on Medicaid is aware of they should re-enroll within the coming months.
Provides Bamberger: “We attempt to unfold the phrase that a very powerful factor is to replace your present data and watch your mail.“
Dominique Jackson in Columbus already filed his Medicaid reenrollment paperwork.
Having Medicaid – and staying enrolled – has turned out to be life-saving for him. Eight months in the past, Jackson was identified with abdomen most cancers.
“I simply went into remission for most cancers final month,” he says. “With out the Medicaid, I do not know the way I’d’ve been in a position to pay – it must utterly have come out of pocket for the value of the medicines and coverings.”
He says this could possibly be his final time counting on Medicaid. He is hoping he’ll quickly be employed on the trucking company the place he is been temping and get on their insurance coverage plan.
[ad_2]
